Increased blood volume during pregnancy increases the quantity of blood being pumped through the blood vessels. Thus, pregnant women may sometimes use aspirin and ibuprofen to address a migraine attack.

However, healthcare providers have to weigh the possibilities that a.
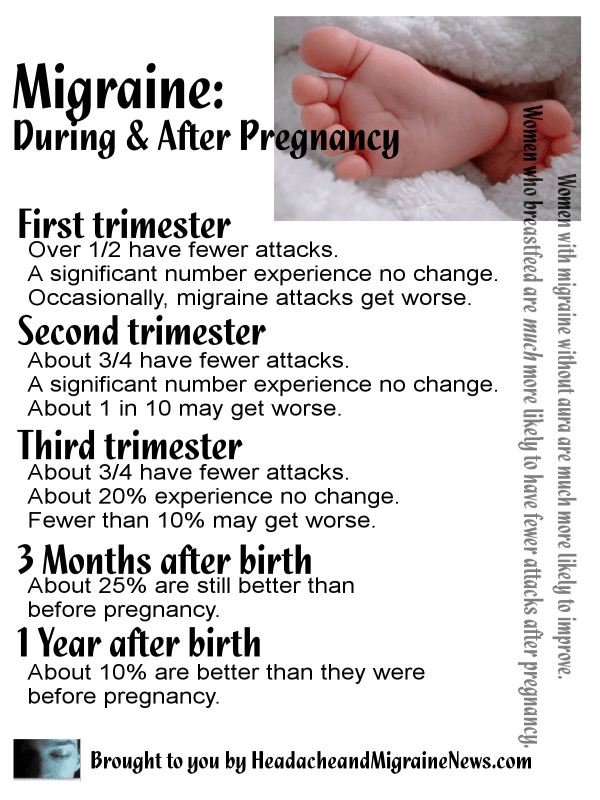
Migraine treatment during pregnancy. If daily medication is considered necessary to prevent migraine during pregnancy, the lowest effective dose of propranolol is the drug of choice.9 low dose amitriptyline is a safe alternative.9 there are no reports of adverse outcomes from pizotifen used during pregnancy or lactation, although it is less often used than the drugs above. It has been estimated that in up to 80% of women who suffer migraines, both the frequency and severity of attacks improve during the second and third trimesters of pregnancy, thus routine prophylaxis with therapies such as topiramate or propranolol is not recommended during pregnancy. What are recommended prescription therapies for pregnant women with migraine?
The location of the injection depends on the type and location of the patient’s migraine. Estrogen is believed to play a role in causing migraines changes in blood pressure : Nondrug therapies (relaxation, sleep, massage, ice packs, biofeedback) should be tried first to treat migraine in women who are pregnant.
Using oxygen and nasal medications for cluster headache. As rachel matured and went through puberty, she found some relief from migraine. Sign, 2018] — regular use should be avoided.
Sign advise use of triptans only where treatment with paracetamol (all trimesters) or ibuprofen (first and second trimester only) has failed. Domperidone and metoclopramide are probably best avoided in the first three months, but this is. The most significant reason for migraine that show up during the initial 12 weeks of pregnancy is the increase in level of pregnancy hormones.
These hormones are several times higher during pregnancy, and though the relief from migraine attacks they provide might last the whole pregnancy, the. Treatment during pregnancy is fairly similar to standard treatment. As suboptimally treated migraine in pregnancy could have negative consequences for both mother and fetus, the primary aim of clinicians should be to provide optimal treatment according to stage of pregnancy, while minimising possible.
Rachel did not experience migraine during pregnancy. Acceptable agents for acute attacks include acetaminophen. Treat migraines in pregnancy, it may be best to consider the safest interventions, which are lifestyle changes likely to reduce the frequency and severity of migraine.
Triptans are recommended as an option for treatment of acute migraine in pregnancy in nice and sign guidance [nice, 2012 (updated 2015); If paracetamol does not provide effective control, Migraine affects up to 25% of women of reproductive age.
However, healthcare providers have to weigh the possibilities that a. Nsaids typically are regarded as the second line of defense against migraine pain during pregnancy. Some have been linked to.
Nerve blocks can give patients relief from migraine during pregnancy. The risks of using aspirin and ibuprofen to treat migraine pain are usually lower than those associated with other types of migraine medications; Prochlorperazine (both the oral and the suppository form) is safe and effective for both nausea and headache.
As a child, rachel seemed to experience migraine attacks during weekends and before exciting events, like a birthday party or sports competitions. For treatment of acute migraine attacks 1000 mg of paracetamol (acetaminophen) preferably as a suppository is. Oxygen therapy was followed by nasal spray sumatriptan and nasal lidocaine, which are pregnancy category b drugs, meaning,.
Increased blood volume during pregnancy increases the quantity of blood being pumped through the blood vessels. The effect of pregnancy on migraine attacks. Like metoprolol, amitriptyline is a medication that could require a higher dose in pregnancy in order to be effective.
Pharmacologic options for treatment of headaches during pregnancy (see table 1 below) are limited and should be avoided if possible. In the majority of these women, migraine improves progressively during pregnancy, but symptoms generally recur shortly after delivery. We believe that opioids and antiemetics are often the treatment of choice for acute migraine during pregnancy whereas that is not the case outside pregnancy.
Migraine is common in women of reproductive age and may occur in pregnancy. Suboptimally treated migraine during pregnancy can negatively affect both mother and fetus, but few data exist on the safety of many. These local injections of a substance like lidocaine or bupivacaine are injected into the scalp to target specific nerves.
Thus, pregnant women may sometimes use aspirin and ibuprofen to address a migraine attack. These include eating regular, healthy meals, adequate sleep, and at least one half hour of exercise (walking is fine) per day. Overall migraine improves during pregnancy especially during the second and third trimesters.